Did you know that approximately 17% of all pregnant women between the ages of 20 and 49 years old are affected by gestational diabetes? It’s true! In this article you will learn what gestational diabetes is, how to treat gestational diabetes, and why it must be taken seriously.
Causes of Gestational Diabetes
Gestational Diabetes is a type of high blood sugar that can affect pregnant women. Researchers don’t yet know why some women struggle with gestational diabetes and others do not, but we do know some lifestyle factors can place some women at a slightly higher risk.
Normally, insulin resistance in pregnant women can begin in the second half of pregnancy. At around the 24th week of pregnancy, the child grows exponentially in size and this can require an increase of up to three times the original insulin requirement. This means that more insulin is needed to transport the sugar into the cells. If the mother’s pancreas does not produce enough insulin to meet this increased need, her blood sugar will rise.

There are factors that increase risk for gestational diabetes:
- Age: >45 years
- Weight: overweight or obesity pre-pregnancy.
- Genetics: immediate family member with gestational or T2 diabetes.
- Ethnicity: Women from the Middle East, South and East Asia (India, Pakistan, Bangladesh) and Africa have an increased risk.
- Previous Pregnancy: The risk increases by 16% if there was gestational diabetes in other pregnancies or very high birth weight babies (> 4500g)
- Comorbidities: Conditions like polycystic ovary syndrome, high blood pressure, or fat metabolism disorders all raise the risk for gestational diabetes.
Uncontrolled gestational diabetes can lead to an increased risk of high blood pressure, urinary tract infections, premature birth, and cesarean section in the mother. Furthermore, maternal blood sugar passes through the placenta to the child. If there is an excess of sugar, the child can become too large for natural childbirth. Likewise, elevated fetal blood sugars can stress the baby’s developing pancreas and boost the risk of the child developing diabetes, obesity, and high blood pressure later in life.
Healthy mother makes for a healthy baby!
Diagnosing Gestational Diabetes
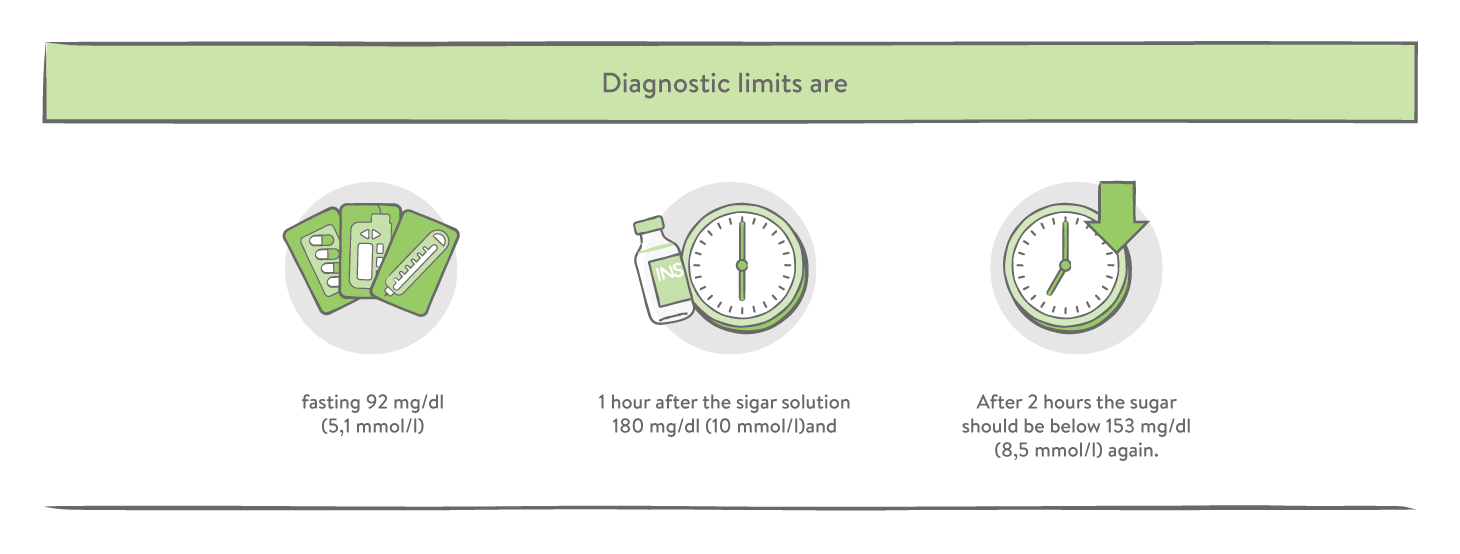
Most pregnant women are offered an Oral Glucose Tolerance Test (OGTT) between the 24th to 28th week of pregnancy as part of standard obstetric care. However, if there are risk factors before pregnancy (see above), the test could be ordered sooner.
The mother will arrive at her healthcare provider’s office and be asked to drink a sugary solution (50 g sugar solution) and wait for one hour. After an hour, a blood draw is done to check the blood glucose levels. If the results are within normal range, then the test is completed. If the results are borderline or even elevated, an additional test can be scheduled to confirm a positive diagnosis.
Treating for Gestational Diabetes
Managing gestational diabetes requires regular blood glucose checks using an at-home glucometer. These are typically readily available at any pharmacy or sometimes even provided by your obstetrician.
Most women manage their gestational diabetes treatment with a healthy balanced diet of 5-6 small meals per day. They choose healthy, high-fiber carbohydrates for good digestion and slower blood glucose impact. Add in some regular physical activity, and many women avoid the need for additional insulin.
For others, insulin is simply a necessity. Either a nightly shot of long-acting insulin to bring fasting glucose levels back to the target area, or mealtime injections of fast-acting insulin might be required. Your individual healthcare provider will guide you on what your glucose levels should be as they may vary with your pregnancy and your baby’s unique needs.
Postpartum
After delivery of the baby, the insulin requirement is usually significantly reduced again and the metabolic state normalizes. This same shift in metabolic state can be expected once breastfeeding ceases as well since that too affects the mother’s hormones.
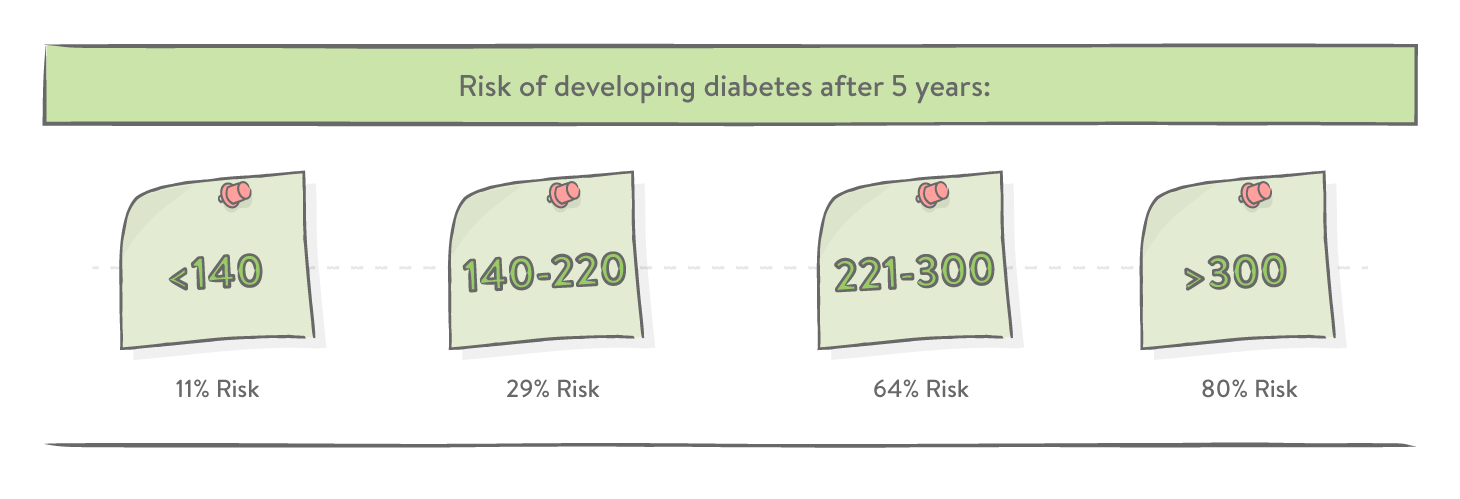
Most doctors do another OGTT at about 6-8 weeks after delivery. If the levels fall within normal range, then the gestational diabetes is resolved and the mother can stop insulin treatments. If the levels are still elevated, then the mother is considered to be one of the roughly 50% of new mothers immediately diagnosed with type 2 diabetes.
The remaining 50% are at higher risk of developing type 2 diabetes for the next 10 years. But it doesn't have to be that way. It is now important to continue eating healthy and keep moving, as well as obtaining regular check-ups with your doctor to watch out for early warning signs of type 2 diabetes. Also, breastfeeding can also significantly reduce the risk.


The mySugr website does not provide medical or legal advice. mySugr blog articles are not scientific articles, but intended for informational purposes only.
Medical or nutritional information on the mySugr website is not intended to replace professional medical advice, diagnosis or treatment. Always consult a physician or health care provider with any questions you may have regarding a medical condition.





