From adrenaline-soaked excitement to prolonged anxiety, stress can have many faces. Sometimes, it can feel like all those stressors don’t play well with your diabetes monster. We’re here to explain how stress impacts your blood glucose and how you can gain control.
Back in our evolutionary history, the original purpose of your stress response was to provide energy reserves for fight-or-flight in case of an emergency. The urban jungle we live in today hardly requires a prehistoric escape, but our body still reacts to our daily stress in the same way it did back then.
And constant, heavy, stress can cause blood sugar levels to rise. But acute stress in certain situations that you perceive as stressful can also cause spikes in your blood sugar levels.¹

Stress Hormones
Stress is the body's method of reacting to threats, challenges, or physical and psychological barriers.² The biophysical response is typically triggered by the autonomic nervous system and can create a cascade of hormones that flood the body including:
- Adrenaline
- Norepinephrine
- Cortisone
- Dopamine²
Because of the autonomic nature of our body’s response, sometimes people can be unaware that they are experiencing a stress response. After all, we release stress hormones when there is a lack of sleep or when we are pressed for time. Being overworked, annoyed, or constantly exposed to excessive noise can even trigger a stress response.³
Unfortunately, these stress hormones make us more resistant to insulin and therein lies the problem for people with diabetes. When stress hormones are involved, most people with diabetes need more insulin to get glucose into the cells.⁴
In addition, more sugar is released from the liver into the blood during stress because our brain needs more fuel to function.⁴ It’s pretty clear how those two processes combined can make managing glucose levels hard for people with diabetes.
Thank goodness for good tech!
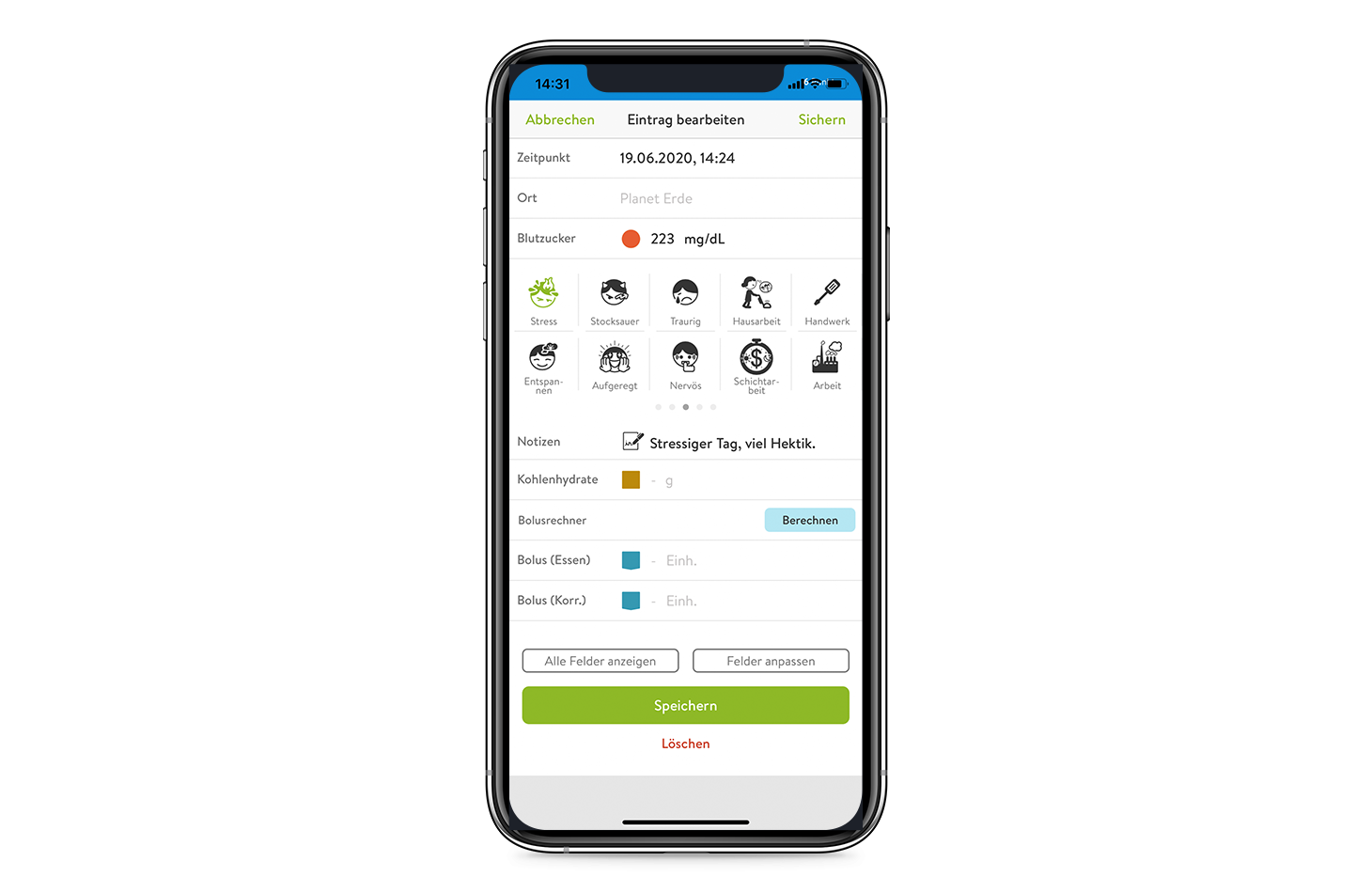
If you enter stress-related glucose values into the mySugr app, and note any stressful events when they occur, it can help you understand your body's unique reaction so you can track trends and alter therapy proactively!
Everyday Stress
These days, stress is so common that literally everyone experiences it.
An exam, an important meeting, an upcoming doctor's appointment, or lingering anxiety, are all things that we deal with on a regular basis. They are so common that sometimes you can look at a wonky glucose value and think, "What's going on with my body?"
You can try relaxation techniques to lessen the physical impact of stress, but sometimes you just need more insulin and that can be tricky with stress-related glucose increases.⁴
“Before my oral exam, I was over 260 mg / dl. When I had this behind me & I could relax, my blood sugar quickly dropped to 108 mg / dl.”
Conny, 39, lives with type 1 diabetes
Again we’ll remind you, stress hormones can cause insulin resistance. So sometimes your standard correction isn’t as effective as you hoped and so you try additional insulin.
The risk here, however, is that glucose levels sometimes stabilize themselves as soon as the stress subsides, and then you are left with too much insulin-on-board and end up fighting a low.⁵
Like a tightrope walk in your diabetes routine. Try to stay calm and check your blood sugar regularly or watch your trend on your CGM if you are using one. Important: Give the insulin its time to work and don’t rush to correct too hastily.
Illness and Stress
The stress response isn’t isolated to just mental or emotional stressors.
Physical illness, inflammation, fever, trauma, and even severe allergic reactions can put stress on the body.³
This is why it is important to discuss insulin adjustments with your doctor during periods of illness. In fact, most healthcare providers have a sick-day protocol that can include:⁶
- Regular blood sugar checks every 2 to 4 hours (and between 2 and 3 o’clock at night).
- In case of fever without vomiting and diarrhea - adjustment of both bolus (rapid) and basal (long-acting) insulin rates may be necessary. Discuss with your diabetes team.
- MDI therapy options can include additional long-acting insulin doses for the duration of illness.
- As usual and discussed with your doctor, correct high blood sugar values with fast-acting insulin. When correcting repeatedly, consider the duration of insulin action and any insulin already working in your body. An insulin calculator (bolus calculator) can help you out here.
- Illnesses that last several days or weeks often require an adjustment of the basal rate. An insulin pump user might require a temporary basal rate adjustment over a few hours or even days.⁶
And of course, all of this illness and additional management of diabetes can be compounded by the hormones created from...you guessed it...stress!
Being aware of how you handle stress during otherwise healthy days can help shape your doctor’s approach to sick-day protocols. So good records can bring better therapy choices!
Note: In the event of vomiting or diarrhea, your values may plummet when losing carbohydrates faster than your body can process them.
And then there are the ketones. If you have type 1 diabetes, measuring ketones in the urine or blood is critical to rule out ketoacidosis.⁷
The Stress-Sleep Connection
Do your thoughts and worries wake you up regularly at night? Do you struggle with insomnia?
Even just one night with a lack of sleep can lead to a reduction of insulin sensitivity.⁸ This can also result in increased feelings of hunger. How much sleep each person ultimately needs is individual.
But a constant lack of sleep can trigger elevated adrenaline levels during the day due to your body needing additional energy to function through fatigue. You should aim for at least 6 hours a night if you can and keep a closer watch on your glucose values during periods of insomnia.
Speaking of sleep. Did you know that weight loss and sleep are connected to each other? According to a study, ample sleep (7-9h per night) compared to a lack of sleep increases the loss of fat tissue.⁹
Stress and Exercise
Because stress is also a reaction to physical challenges to the body, it’s not a big leap to understand how exercise can trigger a stress reaction.
Even the fun, ballistic-style, exercises like intensive cross-training sports can lead to an "adrenaline rush." But low-impact activities like yoga, spinning, or swimming, can lead to smaller spikes in hormones.
With almost any exercise, the body often switches to stress mode. This can cause blood sugar to rise in the short term - whereas endurance sports, provided that your body has already adapted to them, do not create stress and can usually lower the sugar significantly.
Tracking your exercise regularly can help you target your trends and proactively adjust your therapies for them.¹⁰
Stress Eating
We mentioned that our brain needs more fuel to function during periods of stress.
In fact, the brain typically needs about 130g / day of sugar, but when experiencing stress, this need can increase up to 180 g per day.¹¹ Do you ever experience food cravings when you’re using your brain intensively? Now you know why!
The brain sends signals for more fuel and typically our liver plays the regulatory role to manage more glucose being released. However, for most people, we also find ourselves grazing and snacking more often which can lead to elevated blood glucose levels and the need for additional corrections.
Don’t Let Stress Rule You
Managing your diabetes can often feel like walking a tightrope. And adding in stress management can feel daunting. But we are here to reassure you, you can do it!
As always, keep calm and regularly check your blood sugar and watch the trends in your CGM. If you take insulin, let it run its course when you make small corrections and avoid the angry bolus. Keep good records, use your mySugr App to track your stressors, and let your coach or doctor guide you on good therapy choices.

Sources:
- Diabetes.co.uk, 2019. Stress and Blood Glucose Levels. [webpage] Available at: https://www.diabetes.co.uk/stress-and-blood-glucose-levels.html [Accessed 20/01/21].
- Ranabir, S., Reetu, K., 2011. Stress and hormones. Indian J Endocrinol Metab, [online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079864/.
- Mind, 2017. How to Manage Stress. [webpage] Available at: https://www.mind.org.uk/information-support/types-of-mental-health-problems/stress/causes-of-stress/ [Accessed 20/01/21].
- Diabetes UK, 2020. Stress and Diabetes. [webpage] Available at: https://www.diabetes.org.uk/guide-to-diabetes/emotions/stress [Accessed 20/01/21].
- Self, 2018. 6 Things That Can Cause Your Blood Sugar to Spike or Drop. [webpage] Available at: https://www.self.com/story/blood-sugar-spike-drop [Accessed 20/01/21].
- Cigna, 2020. Sick-Day Guidelines for People With Diabetes. [webpage] Available at: https://www.cigna.com/individuals-families/health-wellness/hw/medical-topics/sick-day-guidelines-for-people-with-diabetes-uq2659spec [Accessed 20/01/21].
- Diet Doctor, 2020. The best way to test ketones in blood, breath or urine. [webpage] Available at: https://www.dietdoctor.com/low-carb/keto/ketone-testing-three-ways [Accessed 20/01/21].
- Mesarwi, O., Polak, J., Jun, J., Vsevolod, P.Y., 2013. Sleep disorders and the development of insulin resistance and obesity. Endocrinol Metab Clin North Am, [online]. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3767932/
- Cedernaes, J., Schönke, M., Westholm, J.O., Mi, J., Chibalin, A., Voisin, S., Osler, M., Vogel, H. Hörnaeus, K., Dickson, S.L., Lind, S.B., Bergquist, J., Schiöth, H.B., Zierath, J.R., Benedict, C., 2018. Acute sleep loss results in tissue-specific alterations in genome-wide DNA methylation state and metabolic fuel utilization in humans. Science Advances, [online]. Available at: https://advances.sciencemag.org/content/4/8/eaar8590
- Harvard Health Publishing, 2019. The importance of exercise when you have diabetes. [webpage] Available at: https://www.health.harvard.edu/staying-healthy/the-importance-of-exercise-when-you-have-diabetes [Accessed 20/01/21].
- Health Central, 2008. The Carbohydrate Brain Fuel Myth. [webpage] Available at: https://www.healthcentral.com/article/the-carbohydrate-brain-fuel-myth [Accessed 20/01/21].
The mySugr website does not provide medical or legal advice. mySugr blog articles are not scientific articles, but intended for informational purposes only.
Medical or nutritional information on the mySugr website is not intended to replace professional medical advice, diagnosis or treatment. Always consult a physician or health care provider with any questions you may have regarding a medical condition.





